The Challenge
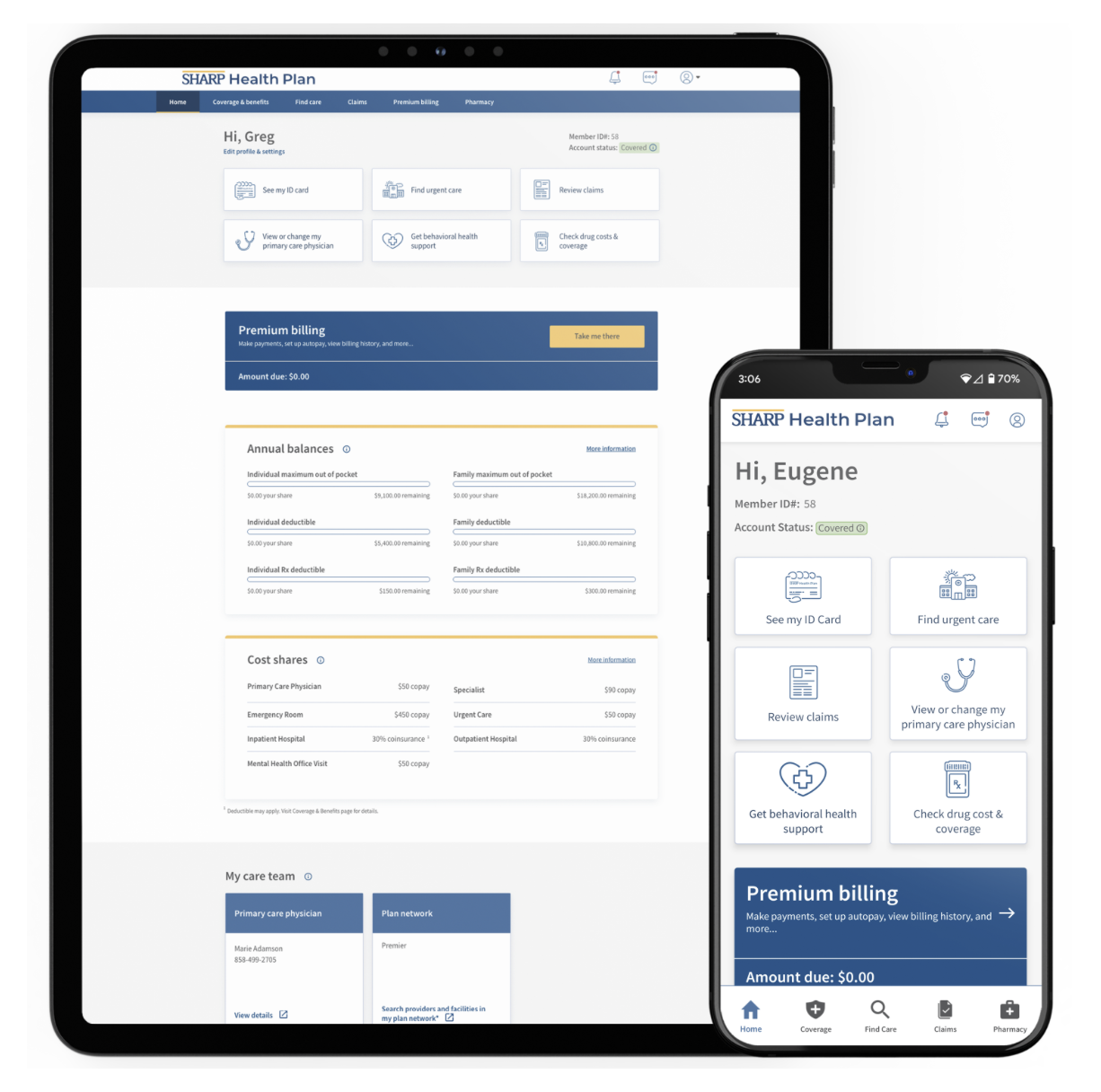
Sharp Health Plan, a non-profit commercial health plan located in San Diego, California, was unsatisfied with the way its customers accessed insurance information. It envisioned enhancing member access to payor information through a custom mobile app and portal integrated with Epic as its foundation. However, the organization recognized a gap in Epic apps’ payor insurance capabilities. Seeking to address this, Sharp Health Plan partnered with Modea to develop a dedicated app and portal. These digital tools seamlessly integrate with Epic and are tailored to include essential plan functions.
Our team worked closely to determine two main goals for this work:
- Provide a high quality mobile app and portal that facilitates care management.
- Offer a personalized consumer experience to advance engagement.
Our Approach
User Experience Research
Modea’s UX/UI team performed an extensive analysis of data provided by Sharp Health Plan. The existing research undertaken by the Sharp Health Plan team led our team to uncover various gaps and challenges customers faced. The research encompassed personas, interviews, and customer care data that indicated the wants, needs, and problems members faced. Sharp Health Plan possessed valuable information, but lacked the resources needed to assemble the puzzle pieces.
Modea expanded its research efforts by engaging with key stakeholders and conducting an industry evaluation. This evaluation specifically delved into the landscape of Sharp Health Plan’s competitors, offering a comprehensive analysis of the user experience and navigation across their respective websites.
We also played a crucial role in crafting personas based on Sharp Health Plan’s primary audiences. This approach facilitated the identification of user flows, enabling us to collaborate effectively with Epic. Through this collaboration, we pinpointed the features to include, identified existing gaps, and explored opportunities for customization.
Ultimately, the research led to the conclusion that Sharp Health Plan members needed a payor app and portal that had EHR integration and customizable features to enhance the user experience.