As healthcare organizations work to modernize patient access, online appointment scheduling has become an important component of the digital patient experience. However, when it comes to integrating scheduling capabilities on a health system’s website, there’s no one-size-fits-all approach. The right solution depends on a health system’s goals, technical capabilities, and operational workflows.
Broadly speaking, there are three common implementation models healthcare organizations use:
- Embedded APIs from EHR Vendors (like Epic MyChart)
- Deep Linking to Specific EHR Endpoints
- Basic Linking to Native EHR Portals
Each of these methods offers varying levels of patient convenience, design flexibility, and technical complexity. Below, we break down what each approach entails, along with key benefits and tradeoffs.
1. Embedding EHR APIs for Seamless Scheduling
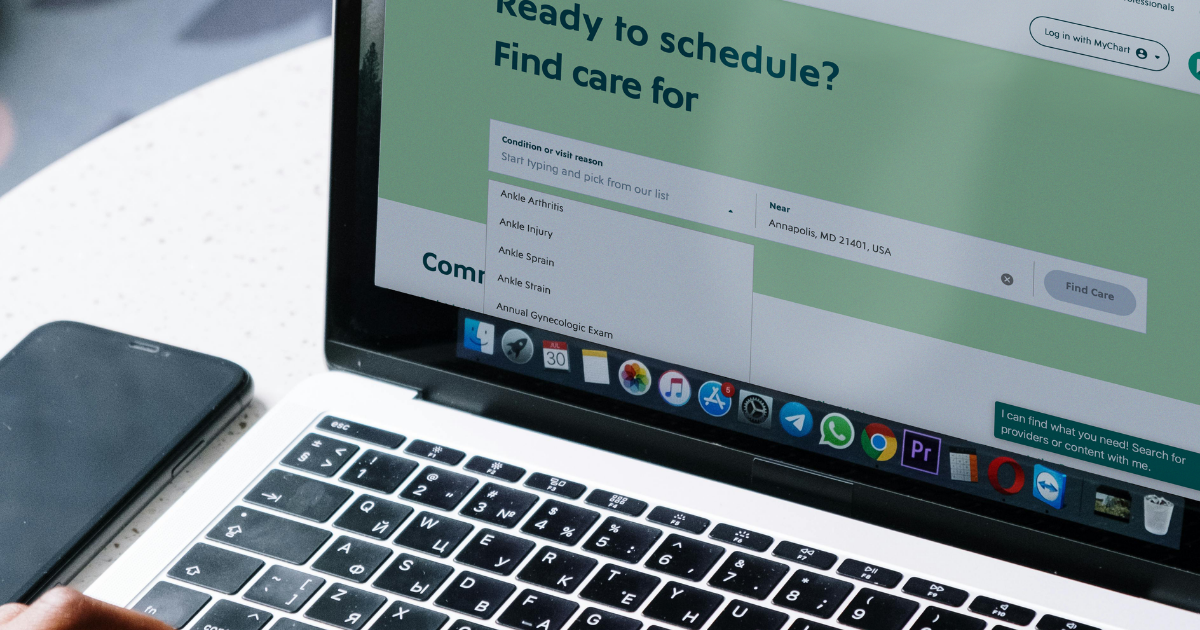
For health systems looking to deliver a cohesive user experience, embedding scheduling APIs directly into their website offers the most streamlined and customizable solution.
In this model, a health system uses APIs provided by its EHR vendor, such as Epic’s MyChart APIs, to allow patients to book appointments without leaving the health system’s website. The API integration can surface available appointment slots, provider information, and even pre-fill user data for existing patients (assuming they have logged in).
This method keeps patients on the main website, preserving branding, UX consistency, and the ability to customize flows. It also enables integration with other digital tools like symptom checkers, provider search, or chatbot triage, creating a unified experience that guides patients from intent to action.
Benefits:
- Consistent, branded UX with minimal redirects
- More control over how appointment options are presented
- Supports integration with other tools such as symptom triage or chatbots
- Improves conversion rates by minimizing friction
- Authenticated experiences enable greater personalization
Considerations:
- Requires close coordination with IT and security teams
- Development and ongoing maintenance can be resource-intensive
- Clinical operations must be aligned to ensure appointments scheduled online = appointments that can operationally happen
- EHR vendor APIs can have limitations or constraints on customization
A health system that took this approach, Luminis Health, saw a 3025% increase in scheduled appointments in 12 months by building a guided, symptom-based scheduling journey on its website using Epic’s APIs.
2. Deep Linking to Specific EHR Endpoints
A middle-ground approach involves designing a patient-friendly scheduling experience on the health system’s website and sending patients directly to a pre-defined MyChart endpoint.
Instead of embedding API functionality into the website, this approach uses customized links that take the patient to a specific scheduling page within the EHR portal, such as a certain specialty, provider, or appointment type.
This model still allows the health system to guide the patient through a branded and thoughtfully designed front-end experience before handing off to the EHR. It reduces the technical lift of full API integration while still improving usability and minimizing steps.
Benefits:
- Easier and faster to implement than full API embedding
- Provides more user guidance than generic links to the EHR home page
- Supports targeted marketing campaigns or search-driven appointment flows
- Reduces confusion by pre-filling specialty or visit type
Considerations:
- The actual scheduling interaction still occurs in the EHR portal
- Design and UX handoff between web and EHR may feel disjointed or inconsistent, potentially disrupting the user experience
- Limits branding and customization once the user reaches the EHR
This approach proved effective for our client, the academic health system Rush. We worked with Rush to launch its “Click for Care” experience that allowed patients to begin their appointment journey on the website with helpful filters and search tools, then transitioned them into Epic MyChart using specific links. Rush saw a 2.5x increase in virtual specialty appointments booked within six months of launch, demonstrating how deep links can bridge user experience gaps without major backend changes.
3. Linking Directly to Native EHR Portals
The simplest and most common approach is linking out to the EHR’s native scheduling portal, typically the MyChart homepage. Many health systems start here because it requires minimal development effort and leverages the functionality already provided by the EHR.
However, this method leaves most of the user experience up to the EHR interface. Patients are often presented with login screens and generic scheduling menus that may not align with the health system’s website branding or design standards. This can create friction or frustration, especially for new patients unfamiliar with MyChart.
Benefits:
- Fast and less resource-intensive to implement
- Maintains backend consistency with existing scheduling processes
- Uses existing authentication and workflows from the EHR
Considerations:
- High drop-off rates due to confusing or non-personalized experience
- Limited ability to guide users to the right care or provider
- Breaks continuity between website and EHR
- Difficult to track user behavior or optimize conversions
While this method may work as a temporary solution or starting point, it doesn’t meet patient expectations for consumer-grade digital experiences and can result in missed opportunities to engage, convert, or retain users.
Choosing the Right Approach: Key Factors to Consider
Each of these three models represents a step forward in digital access, but they also represent a spectrum of trade-offs between speed, customization, and effort.
When evaluating which approach is best for your organization, consider these factors:
- Digital Maturity: Are your website, EHR, and IT infrastructure capable of supporting APIs or deep integrations?
- Patient Needs: Do your users require symptom-based guidance, or are they typically returning patients with specific providers in mind?
- Operational Readiness: Can your call centers and internal teams support a higher volume of self-scheduled visits?
- Strategic Goals: Are you trying to drive volume, improve usability, or modernize your digital experience?
A phased approach is often effective, starting with deep linking or simple EHR links while laying the groundwork for a more robust, embedded API experience.
What all approaches need to keep in mind:
Jae Chong is a Senior Software Engineer at Modea who has helped implement EHR integrations for several clients. He spoke to the need for simplicity and usability of digital tools to improve patient access. “Too often, devs and stakeholders focus on making the tool flashier or adding more features. We sometimes forget that not everyone is tech-savvy or familiar with managing care online. We should keep in mind the 70-year-old retiree using a new smartphone. Or a single parent juggling jobs, childcare, and other household responsibilities who won’t necessarily have time to sit down to go through hoops to set up an appointment for their sick child.”
The reminder to simplify is essential for any approach to implementing online scheduling, as ensuring an accessible and straightforward experience will help maximize patient engagement and success.
Conclusion: Choose the Best Path for Your Organization
Today’s patients expect appointment scheduling to be as intuitive as booking a haircut or dinner reservation. But for many health systems, legacy systems, security concerns, complex clinical and operational workflows, and organizational silos limit that kind of simplicity.
The good news is there are multiple ways to improve online appointment scheduling, and each one moves the needle toward a better, more connected experience. Whether you choose to embed APIs, implement deep links, or simply improve the look and feel of how you connect to the EHR, the goal should remain the same: guide patients to the right care.
As health systems evolve their online scheduling capabilities, the most successful strategies will prioritize patient needs while aligning with backend realities.
