By nearly every objective measure of health, people who live in rural areas are doing worse than those who live in urban and suburban areas.
This health gap between rural and non-rural has persisted for many years. It’s an area of focus for many hospitals and health systems, who are leveraging every digital and analog tool at their disposal to close the gap.
Your digital customer-facing platform can be one of those tools.
In fact, digital investments can help healthcare providers advance health equity by improving access to care for many underserved populations, including rural communities.
But first, you have to understand who your customers are. With hospital consolidation, patient populations are rapidly changing and expanding, and service areas are becoming larger.
In this report, we’ll share some surprising findings about healthcare customers who live in rural communities. And then we’ll help you interpret what these data points might mean for your hospital or health system.
What We Know About Health in Rural Communities
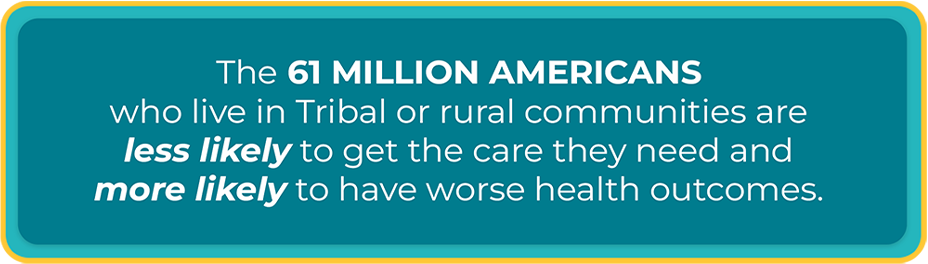
When compared to those who live in less geographically isolated areas, the 61 million Americans who live in Tribal or rural communities are less likely to get the care they need and more likely to have worse health outcomes. They have an increased risk of heart disease, stroke, cancer, and lung disease, and have a higher risk of dying by suicide or having substance use disorder.
Too often, rural residents don’t get the care they need, when they need it. In fact, that lack of access to quality healthcare is one of the biggest contributors to the increased risks and poor health outcomes for rural Americans.
Shortages of doctors and hospitals in rural areas only widen the gap, with two-thirds of hospital closures in the last decade happening in rural areas. Not only that, just 12% of physicians practice in rural communities, where there are also shortages of nurse practitioners, dentists, and social workers.
Hospitals and health systems want to solve this problem. From sponsoring public health initiatives to applying for Critical Access Hospital status, these organizations are leveraging various tools to help address health inequities in rural areas.
However, as a health system or hospital, you have another very powerful tool: Your website and mobile experience.
The Data in This Report
Our clients—which include local, regional, and multi-state health systems—often cite improving access to care as one of the reasons they are investing in digital. But what does digital access look like for people who live in rural areas?
To answer that question, among others, we recently conducted independent research, surveying more than 1,200 individuals across the U.S. We wanted to learn more about how they access care, and what keeps them from accessing care. We also combed through other research on healthcare access for rural Americans.
What we gleaned can help hospitals who are seeking to better serve those who live in geographically isolated areas.
The Big Idea
Investing in and improving customer-facing digital tools can increase access to care for many underserved populations, including rural communities.

Key Finding #1: Rural Users More Likely to Rely on Smartphone, Less Likely to Have Computer
In our survey, about 90% of respondents living in rural areas reported having a smartphone.
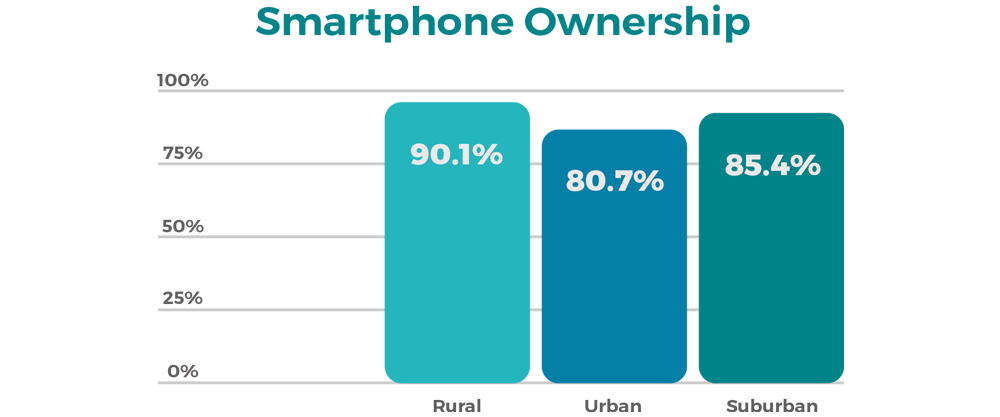
Surprisingly, smartphones were more common among rural individuals (90.1% ownership) than urban (80.7%) or suburban (about 85.4%).
Individuals living in rural communities were the least likely to have either a desktop computer or a laptop computer (while 79.8% reported owning one or the other, only 45.8% of rural Americans reported owning a desktop computer). A 2021 Pew Research Center survey confirmed this, finding that while smartphone ownership had increased significantly over the last 3 years, ownership of desktop or laptop computers stayed flat.
These two points together mean that rural users are most likely to use their smartphone when searching for care, and least likely to use a computer.
For this reason, the healthcare websites most accessible to rural users are those built to be mobile first. This means that the design and function of the website is built thinking of mobile first, and desktop second.
Key Finding #2: People Living in Rural Areas Are Less Likely to Have Broadband Access
Compared to those living in urban or suburban areas, rural individuals are nearly two times more likely to lack broadband access.
A Peterson Center on Healthcare and Kaiser Family Foundation report found that, in 2019, 13% of people in nonmetropolitan areas lacked internet access at home (compared to 7% of people in metropolitan areas).
Not only does this finding underscore the point that mobile-first matters for rural users, it also is a reminder that not all users with a smartphone have internet access. This is another reason why they tend to be smartphone-dependent.
Furthermore, if they are leveraging a cellular network to connect, their page load times will be longer. The longer the page load time, the higher the bounce rate tends to be.
This is why it’s important to work with UX designs and web engineers who know how to design and build for optimal page load time.
It’s also an important consideration for telehealth, in that you have to understand how your users will connect and what types of technology are most accessible over cellular networks.
Key Finding #3: Rural Users Are Willing to Drive
When we asked about barriers to care, rural respondents were slightly more likely to cite issues with work and childcare than urban and suburban ones. But surprisingly, they were less likely to flag transportation or distance as barriers, compared to urban individuals.
One explanation is that people living in urban areas may be less likely to have a car, and if the subway or bus line isn’t near where they go for care, it limits them.
We do have to acknowledge that much research has focused on the travel burden for people living in rural areas, with one study finding that rural residents traveled more than twice the distance (nearly 18 miles) as urban residents (about 8 miles) for healthcare. In that same study, more than 55% of rural residents identified the cost of gas and the financial expense of travel as barriers, compared to 45% of urban residents.
But what our data suggests is that a hospital’s service area may be larger than they think. This is especially true with hospital acquisition and consolidation. People living in rural areas may be willing to drive further—even to the next hospital over—if they think the care is better or if booking an appointment from their phone is easier.
Hospitals must be aware that their competitive set is becoming broader, which has strong marketing implications. Are you really reaching your full demographic?
Key Finding #4: Rural Users Most Likely to Use Family for Finding Care, But Also More Likely Than Other Cohorts to Use App
We asked respondents a series of questions about how they prefer to research a condition and how they prefer to find care.
Rural residents are the most likely to want to talk directly to their doctor, both to find care and to research care. They are also the most likely to turn to family for both things. This suggests they put their faith in people over technology, which makes sense if we think about rural individuals living in small, tightly knit communities. They value personal connection when making healthcare decisions.
However, they are almost as willing as other cohorts to use Google or a hospital website for researching care. And most interesting, rural users were more likely than either urban or suburban users to use an app to find care. That said, they are less likely to use an app to research care, preferring to turn to people for help making decisions. In essence, they are the happiest of all the cohorts to use an app to make an appointment – or to leverage technology to get in front of a provider as quickly and efficiently as possible.
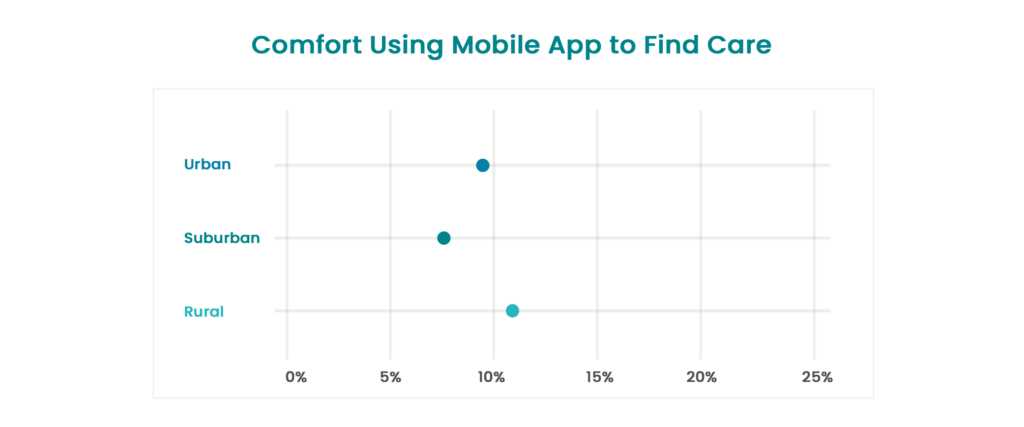
Building a proprietary hospital app is a significant digital investment, but it gives hospitals complete control over the digital experience, allowing them to customize for their customers.
We know from previous research on customer preferences regarding hospital apps that convenience and ease of use are the top factors. And the way to ensure your customers can do the key tasks they care most about is for your hospital to own the app, just like any other digital property.
Key Finding #5: Telehealth Has Vast Potential for Rural Communities
The Covid-19 pandemic dramatically increased the number of people using telemedicine. For people living in rural areas, telehealth can be a more accessible way to talk to a provider. A 2022 study showed that people in rural areas have strong interest in telemedicine and mostly positive experiences.
In fact, the CDC is supporting specific telehealth projects in rural areas, including stroke and cardiac rehab, diabetes prevention and management, tobacco cessation, and epilepsy management.
Building a sustainable telehealth platform can involve regulatory and operational challenges for health systems, and it brings up many questions. Do you have providers who will offer video visits? Do you have the security you need to keep visits compliant? And for rural users, a big watchout is making sure the platform is set up in a way that allows them to access from mobile only.
For hospitals and health systems reaching rural America, telehealth should always be part of the digital discussion. In other words, if you’re investing in your digital platform and you’re not even talking about how to integrate telehealth, you’ll find yourself behind the curve.
Where Do We Go From Here?
At Modea, we believe in the power of a terrific digital customer experience. We work toward creating these experiences for our hospital and health system clients because we believe digital can improve the consumer experience and make healthcare more human and personal.
But we also believe Americans need better access to healthcare. And building great digital tools that improve access is the difference we can make.
This is why we want to make sure that hospitals and health systems know the opportunity they have to reach people in rural areas.
Not sure where to start? We recommend that hospitals work to gain clarity on these 3 things.
- Know your customers. Has your service area expanded in the last few years? We see this with our health system clients who are buying hospitals or consolidating. If it’s been a while since you’ve done Voice of the Customer research or mapped your customer journey, now is the time. (Learn more about what digital roadmapping looks like.)
- Know what your data is telling you. Do you understand how customers in different zip codes are interacting with your digital properties? Do you know what devices they are using to access your website? Do you know where they are getting lost in the process and where they are converting? Your data tells a powerful story, if you know where to look. (Learn more about the analytics and BI work we do.)
- Know where the gaps are in your digital tools. If you haven’t audited your digital tools with an eye toward access to care, particularly for historically underserved populations, you likely don’t know what you don’t know. Talk to us today about a Digital Equity Audit.
Sources:
- Addressing Rural Health Inequities in Medicare. CMS.gov blog.
- Some Digital Divides Persist Between Rural, Urban, and Suburban America. Pew Research Center.
- Healthcare Access in Rural Communities. Rural Health Information Hub.
- How Might Internet Connectivity Affect Health Care Access? Peterson-KFF Health System Tracker.
- Do Rural Residents Experience Great Travel Burdens in Accessing Healthcare? Rural Health Info.
- Telehealth in Response to the Rural Health Disparity. Health Psychology Research.
- Telehealth in Rural Communities. Centers for Disease Control and Prevention.